


Palliative care, as described by the WHO is 'an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.’
‘Total pain management’ is the core responsibility of a family physician, he / she being in touch with the entire family and knowing each member better than any other practitioner.
The GP is in a unique position , especially in the context of managing chronic pain which the palliative care worker encounters very often.
Good pain management depends on the following principles:
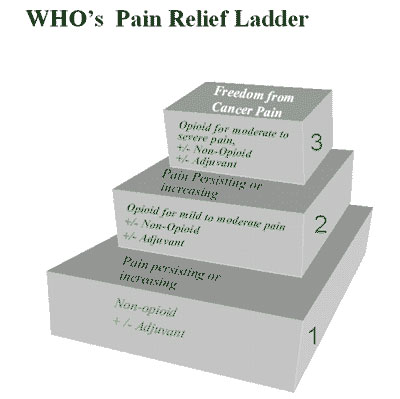
1. Making a pain diagnosis, mostly by relying upon on a good pain history and observation 2. Pain assessment 3. A step ladder approach to the use of analgesia based on WHO Analgesic Ladder 4. Monitoring and follow-up A pain diagnosis is made on the basis of International Association for Study of Pain (IASP) pain definition which states that "Pain is a subjective, unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.
The pain history is summarized based on "PQRST":
Palliative /provocative factors Quality /character of pain Radiation of pain Severity of pain Time – i.e. diurnal variation
The pain history will reveal whether the pain is of somatic, neuropathic or mixed origin. Severity of pain can be assessed by using pain assessment tools like Wong-Baker's Faces Pain Scale, Numerical Pain Scale and FLACC scale(Face, Legs, Activity, Cry, Consolabilty scale). Accuracy of the scale and getting a good assessment comes with follow up and taking the whole concept of "total pain." Pain is not just physical alone but mental, social and spiritual. In other words, it is described that pain is a psychosomatic phenomenon modulated by mood, meaning and morale of the patient.
A good pain assessment is followed by the proper implementation of WHO Analgesic Ladder. Over 80-90% of the pains can be controlled with WHO Analgesic Ladder. The basic rules are:
5. Follow up of pain management is a must, just as any other symptom management. It is necessary to assess the adequacy of analgesia, monitor and treat the unwanted side effects of drugs, aggravation or onset of any other pain. Difficult to control pain might be due to multiple pains, unaddressed aspects pain like hopelessness, helplessness, insomnia, exhaustion, depression, anorexia and fatigue.
To conclude, a successful pain management must have the characteristics of ABCDEF of pain management.
Palliative care has evolved into a new speciality in clinical medicine. Therefore, it is mandatory that a family physician possesses competency and skill in the management of chronic pain. The concept of cure sometimes, comfort often and care always, should be a stepping stone to improve the quality of life of the patient with chronic illness/pain. Finally, caring for people who are dying is challenging but very fulfilling at the same time. After all dignity at death and positive memory for those who live on, is the work of angels. And being a part of angelic work is a wonderful feeling.
“I wouldn't want to die alone but with at least an angel by my side when my time comes finally”.
| YOUNG DOCTORS MOVEMENT |STATE LEADERS | FMPC 2019 | FMPC 2020
| AFPI
© All rights reserved 2020. Spice Route India 2020
Contact us at TheSpiceRouteIndia@gmail.com