


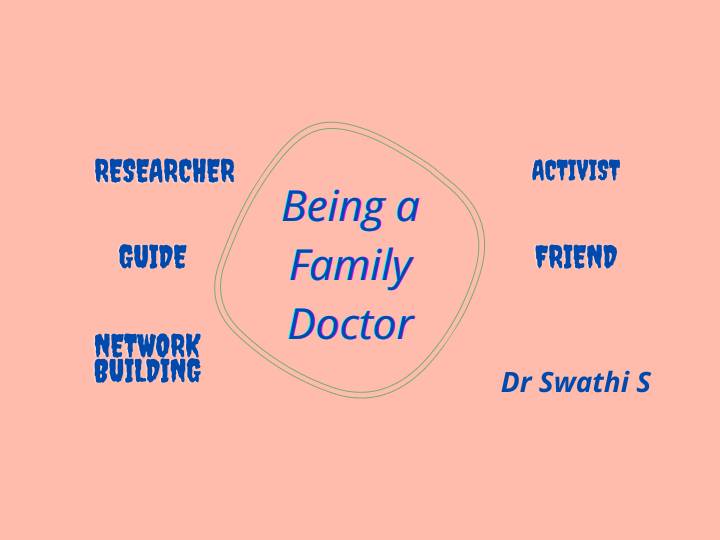
In my opinion, a family doctor is a leader first and a doctor next. For effective patient care and practice, a practitioner needs to build a team, figure out finances, market the practice, ensure right partnerships for the patient care. We treat, talk, train, write, research, advocate, make mistakes and learn from them, adapt, improve, and make lives better.
I would like to highlight some of these aspects through the following practice reflections:
Our early education has in some way made us think that a practitioner is supposed to know it all. Examinations are very individual focussed. But in real-world practice, delivering primary care to people is much more complex, often requiring its own teams, working with other local practitioners and hospitals. Involving the right partners in the care often brings about better results where care not only involves medical but social health as well. Last week a lady called to see me for the first time who had travelled back to Bangalore. She is known to have HIV infection, and was under regular treatment. She sounded very sick (probable ART failure). By the time the appointment could be fixed, she had severe vomiting and hence approached a hospital nearby and got admitted. The hospital was kind enough to admit her without much hassles related to COVID 19 testing. So I spoke to the treating doctor to understand the condition, and we discussed the plan of management where both the treating doctor and I benefited from the discussion which would help in patient care. Later that day, I visited her in the hospital and we planned to care for her further with help from an NGO. This made me realise that professionals are open to working together. We just need to reach out, keeping our patients in the centre of our thinking. The doctor also mentioned that in future our clinic team can admit our patients if we wanted and take care of them in their hospital as consultants. Building such relationships enhances both patient care as well as our professional growth and practice.
A 35 years old lady came with generalised weakness, tiredness and difficulty in concentrating. She had burn marks over quite a large extent of her visible skin ,her neck and both forearms
. Kathryn Harrison once remarked, “Scars are stories, history written on the body”.
As I probed further, and she became comfortable with me, she started narrating the domestic abuse that she was subjected to, as a child, by her mother and now by her husband. Her husband is dependent on alcohol, and abuses her, which was why she had set herself on fire 5 years ago. It seemed that she hadn’t reached a point where she had decided to leave him or take any action towards this.
I had to pause a bit to digest this. I have heard hundreds of stories like this from papers, people, TV but I always dreaded the time when I would come across it during practice. I realised I had several resources to deal with this. I knew the organisation she was working with and decided to take their help. We agreed to tackle her issues in a multimodal fashion. I started her on symptomatic medications and linked her to tele counselling services to assess and address her mental health status. Meanwhile, I discussed with the organisation lead and came up with a plan where we used 'women's group sharing' as a platform for empowering her to take further decisions on the course of action and support her with those decisions. Staying in touch with her and seeing her go through this phase became easy with the involvement of the right partners. And I’m sure her weakness will fade with time.
A few days ago, I heard from my practice group that they helped a pregnant lady, who went into labour, and was advised to get COVID 19 testing done before she could get admission to a hospital! This is after having to run across 8 hospitals (both public and private). This story is not entirely unheard of. Even before the pandemic, women in rural areas have faced this situation. But this story and other recent news reports about this situation happening across the country, even in metro cities, due to hospitals making it mandatory for COVID 19 testing before admission seemed unacceptable.
As a family practitioner, our first response is definitely to ease the process for the patient by figuring out the best way to get the test done so that the mother and the baby remain safe.
But there are hundreds of such women who might not have such teams to fall back on to seek help. Don’t we as practitioners have the responsibility and to a certain extent, power, to vouch for our patients, for ensuring quality care? We might be at the right place to do so than many others not involved in patient care, because we are the system.
In the above situation, we made a petition on the website 'change.org’. We are also in the process of releasing a statement with people’s endorsement for demanding the government to take necessary action to stop this. Is this politics? May be. If we reflect upon this, every citizen and even more, the doctors, cannot escape being a part of this on a daily basis, since what happens through the government or the court affects our profession and our patients.
So as a family practitioner, I stand up for my patients. Even if it is as simple as talking to the lab in-charge at a diagnostic centre who forced my patient to reveal their HIV status and made them uncomfortable. I will definitely make an attempt to change this attitude. Family practitioner as a researcher
For constant growth of the practice and quality improvement, research cannot be separated from practice. Local and contextual knowledge generation is the way forward for improving evidence.
Research in practice need not always involve complex methodologies, funding, and teams. Many benefit by being inquisitive and sharing the practice lessons. It could be in the form of writing, synthesising, documenting, looking at patterns, discussing with peers and experimenting. Questions like - why are my patients not responding well to this drug, which is known to be effective? What are the reasons for not achieving good glycemic control in certain patients? What is the next best investigation/ management plan if a certain diagnostic test is unavailable or diagnosis is unclear?
These are the elements that actually make family medicine practice rich, challenging and highly meaningful. We are the doctors who stand by our patients and not just treat their illnesses. We are the “go-to person” for advice. We are privileged to having information that they might not have shared with anyone else. That’s what makes our practice special and deeply personal.
To summarise,
We graduate from MBBS and residency often with good clinical mentorship: the differential diagnoses, the drugs, their side effects and how to manage them, specific areas to look for cardiac murmur and what we infer about the specific heart condition the person might have. It’s only after this formal education that we realise practice in community settings involves so much beyond this, especially when you are a family physician or a primary care physician and want to make a difference in the lives of others. The current pandemic has only made this brutally clear.
Dr Swathi S Balachandra
PCMH Restore Health, Bangalore.
| YOUNG DOCTORS MOVEMENT |STATE LEADERS | FMPC 2019 | FMPC 2020
| AFPI
© All rights reserved 2020. Spice Route India 2020
Contact us at TheSpiceRouteIndia@gmail.com